Could Oligomannate be a new Alzheimer’s treatment?

The impact of Brexit on Dementia
October 15, 2019
Dementia-Friendly Christmas
December 17, 2019Could Oligomannate be a new Alzheimer’s treatment?
Jennifer Pinnell
On Saturday 2nd November 2019, China’s National Medical Products Administration (NMPA) approved Oligomannate as a new oral treatment for mild to moderate Alzheimer’s disease. The developers of the treatment, Shanghai Green Valley Pharmaceuticals announced the approval with much excitement, however the worldwide scientific community suggest caution until we understand more about how the treatment may work.
As the first new Alzheimer’s treatment to be granted approval since 2003, there is great excitement about the potential of Oligomannate to improve the lives of Alzheimer’s patients.
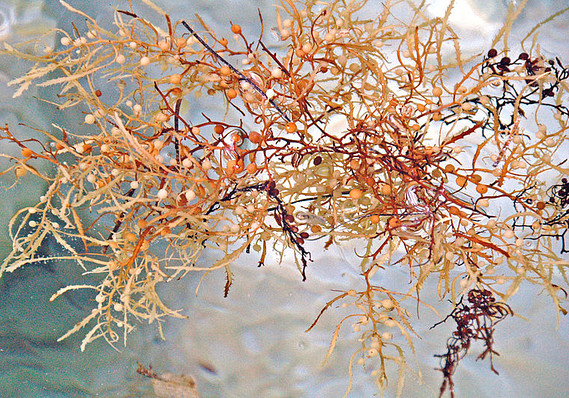
Oligomannate is derived from an extract of marine brown algae and successfully passed a Phase III clinical trial prior to approval. The randomised, multicentre, double-blind placebo-controlled trial, which lasted 9 months, included a total of 818 patients who were either given 900mg Oligomannate or a placebo twice a day for the trial duration. The patients, who were assessed to have mild to moderate Alzheimers, were randomly assigned to a group, with their doctors only discovering who was in which group after completion of the study to avoid introduction of bias in the results.
The primary research outcome of the trial was to measure cognitive changes using the Alzheimer’s disease cognitive subscale, which involved evaluating each patient on seven performance tasks including memory, orientation and language. The doctors also monitored for changes in the patients mood, agitation, psychosis, attention, concentration and weight.
Although the results from the study have yet to be published in a peer-reviewed journal, Green Valley reported that Oligomannate significantly improved cognitive function as early as 4 weeks after treatment initiation, with sustained efficacy throughout the trial. The drug was considered to be safe and well tolerated in patients, with reported side effects comparable to the placebo.
These results are very exciting, as there are currently a limited range of drugs available to treat Alzheimer’s disease, with none which can delay or prevent the progression of the neurodegenerative disease.
It has since been announced that Shanghai Green Valley Pharmaceuticals expect Oligomannate to be available to patients in China by the end of the year.
For the rest of the world, further trials will be needed to confirm that Oligomannate is as effective as this first trial demonstrates and to help us better understand how it functions to protect against cognitive decline. Trials in Europe, the US and elsewhere may begin as early as 2020, which could lead to approval of Oligomannate for use in these countries if they are successful.
The current theory is that Oligomannate works by altering the bacteria which live in our guts (called the microbiome), to reduce the amount of harmful products they produce. This seems to reduce inflammation and reduce the build up of harmful proteins in the brain, which are believed to contribute to the progression of Alzheimer’s disease. Without the publication of the Chinese Phase III study data for scrutiny, we are unable to develop any certain theories about how Oligomannate may function.
The microbiome is different in each individual, as it can be affected by our diets, where we live and any infections or treatments (such as antibiotics) which we may have had. This means that Oligomannate may prove to be more effective in some populations than others due to natural variation in the microbiome, if this is how it functions.
Along with validation of the drugs mechanism of action, further trials would need to assess the long term safety and efficacy of Oligomannate as a treatment; if approved, patients could be prescribed Oligomannate for long term use so we need to be certain of its safety for treating patients for longer periods of time.
The microbiome and changes in the gut have also been implicated in other neurodegenerative disorders, including Parkinson’s disease, in which build up of toxic protein in the gut neurons is believed to precede its accumulation in the brain where it leads to death of important neuronal populations. As this drug may function by a different mechanism to many Alzheimer’s drugs, it may also be applicable to other neurodegenerative diseases and lead to improved treatment for more than just Alzheimer’s patients.
Only time and further research will tell whether this could be a fantastic new treatment or whether the results are being overstated and the wait for new treatments will continue.


